Understanding Blood Donation
Blood donation is a crucial medical intervention that saves numerous lives worldwide. The process involves collecting blood from a donor to be used for transfusions or made into biopharmaceutical medications. This article explores the scientific principles underlying blood donation, shedding light on its importance and the processes involved.
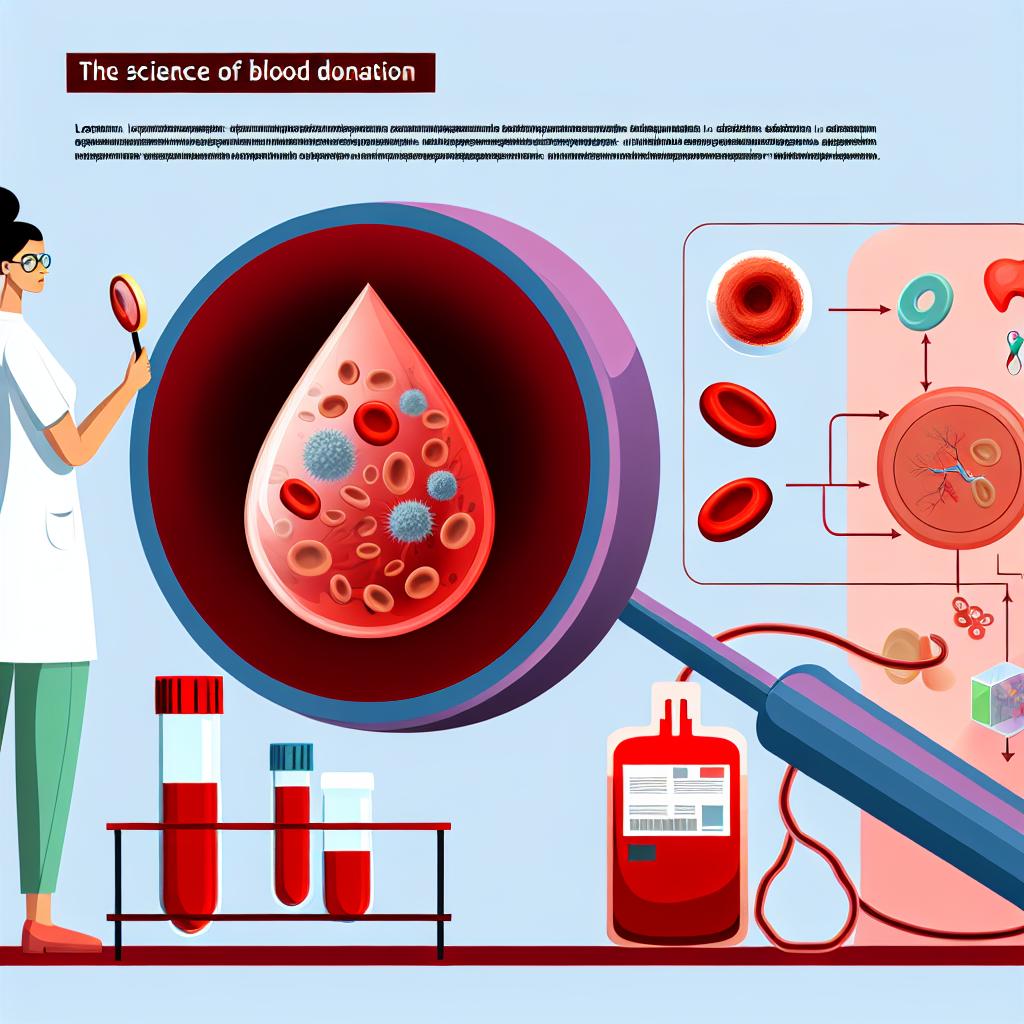
The Composition of Blood
Blood is a vital connective tissue composed of plasma, red blood cells, white blood cells, and platelets. Each component plays a distinct role in maintaining physiological balance:
Plasma: This is the liquid component, making up about 55% of blood volume. It is primarily composed of water but contains vital proteins, glucose, clotting factors, electrolytes, hormones, carbon dioxide, and oxygen. Plasma serves as a medium for transporting nutrients, waste products, and other substances throughout the body. By acting as a conduit, plasma plays a key role in regulating body pH and temperature, offering a stable environment for cellular functions.
Red Blood Cells (RBCs): These cells are responsible for carrying oxygen from the lungs to the rest of the body and returning carbon dioxide to the lungs for exhalation. RBCs give blood its characteristic red color due to the presence of hemoglobin. Hemoglobin binds oxygen molecules in the lungs and releases them where they are needed in the body’s tissues, playing an essential role in sustaining life by maintaining efficient oxygen delivery systems.
White Blood Cells (WBCs): As part of the immune system, WBCs help fend off infections and play a key role in the body’s defense mechanisms. Each type of white blood cell, such as neutrophils, lymphocytes, and monocytes, performs distinct functions ranging from pathogen destruction to antibody production. Their presence in the blood is crucial for quickly responding to infections and fostering long-term immunity.
Platelets: These small cell fragments are crucial for blood clotting, which prevents excessive bleeding in case of injury. When a blood vessel is damaged, platelets form plugs that help seal the wound. Additionally, they release chemical signals that initiate and regulate the blood clotting cascade, ensuring that bleeding is effectively controlled and tissues are protected from further damage.
The Donation Process
Understanding the blood donation process helps demystify the experience for potential donors. Here is an overview:
1. Pre-Donation: Prospective donors are required to complete a health questionnaire and undergo a brief physical examination. This step ensures the safety of both the donor and recipient by identifying any conditions or factors that may pose a risk. The screening process typically evaluates iron levels, blood pressure, and hemoglobin content to ensure donors can safely give blood.
2. The Donation: During the procedure, a sterile needle is used to draw blood, typically from a vein in the arm. The process usually takes about 8-10 minutes, during which approximately one pint of blood is collected. This amount constitutes about 10% of an average adult’s blood supply, which can be replenished quickly. The process is designed to be as comfortable and efficient as possible, with trained staff ensuring a smooth experience.
3. Post-Donation: Donors often receive refreshments to aid recovery. It is recommended to rest briefly and avoid strenuous activities for a short period after donation. Consuming fluids and iron-rich foods can further support recovery, as they help replenish what the body has donated. The post-donation guidelines are a critical part of ensuring donor well-being and encouraging future donations.
Types of Blood Donations
There are various types of blood donations, each serving different medical needs:
Whole Blood Donation: This is the most common type, where donors give about one pint of blood. It is often used in trauma cases and surgeries, where a complete blood supply is needed to support various functions in treating patients.
Apheresis Donation: This technique involves the separation of blood components. Donors can give specific components like plasma or platelets, while the remaining blood is returned to the donor’s body. Apheresis allows for the collection of high quantities of specific blood components that are in high demand, such as platelets for cancer patients undergoing chemotherapy.
Autologous Donation: Individuals donate their own blood for their future use, often before undergoing planned surgeries. This ensures compatibility and reduces the risk of transfusion-related complications during medical procedures, making it an appealing option for those with rare blood types or specific medical concerns.
The Science of Compatibility
Blood transfusions depend on compatibility between the donor’s and recipient’s blood types, primarily determined by antigens present on RBCs. The widely known ABO blood group system, along with the Rh factor, plays a significant role. Mismatched blood transfusions can lead to severe immune reactions, highlighting the importance of meticulous blood type matching.
Understanding the ABO blood group system is crucial as it categorizes blood based on the presence or absence of antigens A and B on the surface of RBCs. For instance, type A blood has A antigens, type B has B antigens, AB has both, and O has none. The Rh factor further classifies blood as positive or negative, depending on the presence of Rh antigen. Ensuring donor and recipient compatibility involves carefully matching these factors to prevent hemolytic reactions that can endanger lives.
Research and Innovations
The field of blood donation has seen continuous advancement. Researchers are exploring synthetic blood substitutes and improvements in storage techniques to enhance the safety and shelf life of blood products. Blood substitutes aim to mimic the oxygen-carrying function of RBCs, potentially alleviating shortages and offering safer options for transfusions.
Improved storage techniques focus on extending the viable period of stored blood components. Breakthroughs such as cryopreservation and pathogen inactivation are paving the way for longer-lasting blood supplies, making it easier to manage inventories and respond to emergencies effectively. Such advancements promise to address challenges associated with blood shortages, enhance safety, and improve outcomes for recipients worldwide.
Conclusion
Blood donation is an essential medical practice that epitomizes the altruistic spirit of humanity. By understanding the science behind it, we can appreciate its significance and encourage more individuals to participate. Raising awareness about the different types of blood components, the donation process, and compatibility issues helps dispel myths and promotes a culture of giving. Creating an informed society where individuals are encouraged to donate not only saves lives but also strengthens community resilience and health systems. For more detailed insights into blood donation, consider visiting the American Red Cross or similar organizations involved in blood services.