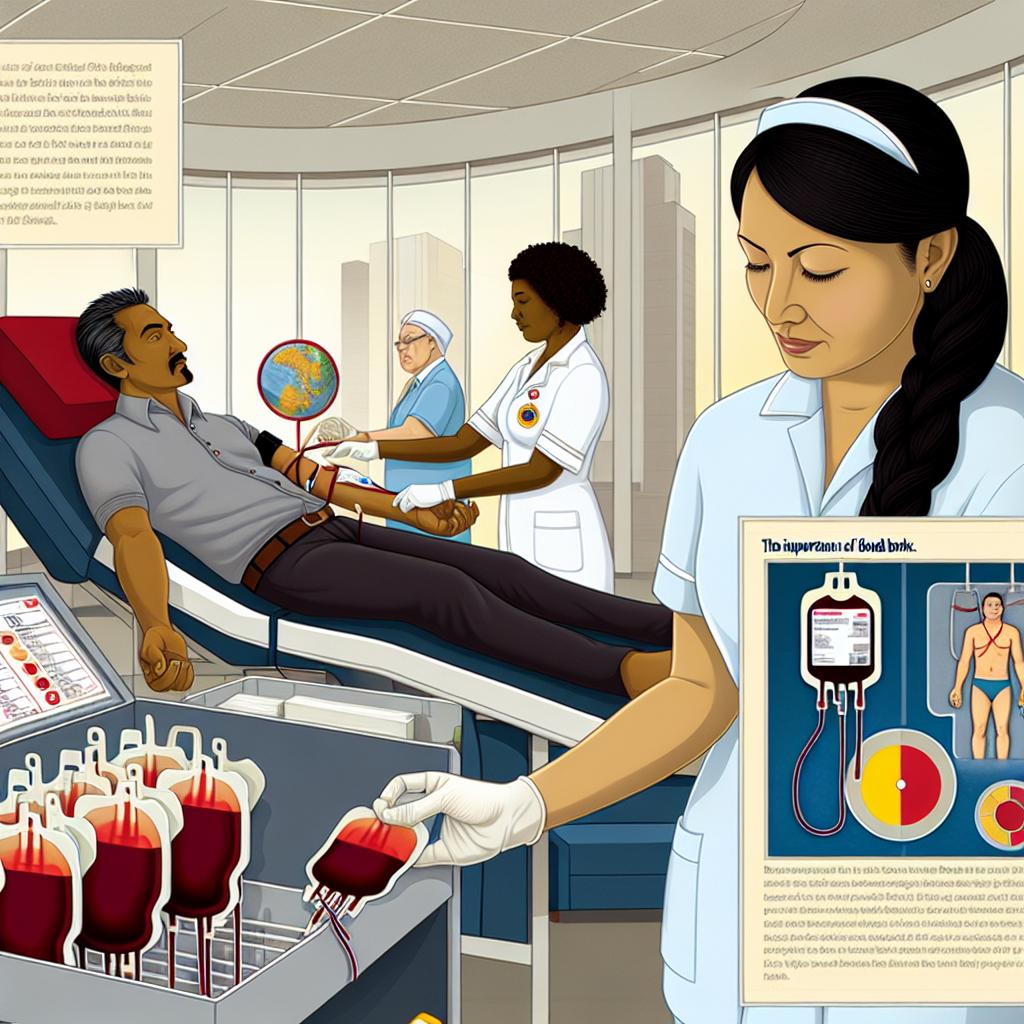
The Role of Blood Banks in Healthcare
Blood banks serve as a cornerstone in the framework of modern healthcare systems. Their primary function is to ensure that blood and its vital components are readily available for transfusions, a necessity that can be the difference between life and death in numerous medical scenarios. Whether it’s for routine surgical procedures or the urgent care required in traumatic injuries, the accessibility to a consistent and safe blood supply is paramount.
Collection and Storage of Blood
Collection Process: Blood banks undertake the responsibility of collecting blood samples from donors, which is a multifaceted process designed to prioritize the safety and effectiveness of the blood collected. The operation begins with the recruitment of eligible donors, ensuring adherence to strict health and eligibility criteria to maintain the highest safety standards.
Component Categorization: Post-collection, the blood is meticulously categorized into various components—red blood cells, plasma, and platelets. Each component plays a distinct role in medical treatments, catering to patients with specific needs. For instance, red blood cells are crucial for those suffering from anemia, plasma supports patients with clotting disorders, and platelets are indispensable for individuals undergoing treatments that impair blood clotting.
Storage Conditions: Once categorized, the blood and its components are preserved under a controlled environment to ensure their viability. Advanced storage techniques are employed, including the use of refrigeration for red cells and specific temperatures for plasma and platelets. Each component has a defined shelf life, necessitating precise inventory management to optimize the use of donated blood.
Types of Donations
The processes of blood donation are versatile, designed to maximize the utility of each donation based on patient needs. These include whole blood, platelet, plasma, and double red cell donations, each serving unique clinical purposes.
Whole Blood Donation
This is the most common form of donation, where donors provide a unit of whole blood. The procedure is straightforward, typically taking about an hour, and plays an integral role in bolstering routine blood supplies. Whole blood donations are versatile as they can be separated into their primary components, expanding the range of applications.
Platelet Donation
Focused on collecting platelets, this method is more time-intensive compared to whole blood donation but no less crucial. Platelets are extracted via a process known as apheresis, leaving the remaining blood components to be returned to the donor. Important for patients whose conditions impair platelet function, such as those receiving chemotherapy, platelet donations are critical for their recuperation.
The Demand for Blood
Blood demand is a constant factor within healthcare due to its limited storage lifespan. Consequently, blood banks must maintain a robust inventory to fulfill the needs of patients undergoing varied treatments, from scheduled surgeries to urgent trauma interventions.
Emergency Situations
Emergencies, such as traumatic injuries resulting from accidents or natural disasters, can drastically increase the need for blood. During such times, the capacity of blood banks to provide immediate and sufficient supplies is vital. Preparedness in such situations demands coordination with health institutions to guarantee that the sudden spikes in blood requirements are sufficiently met.
Safety Measures and Screening
The safety of the blood supply is a non-negotiable aspect of blood banking operations. Each donation undergoes stringent screening procedures, crucial for identifying infectious agents that could pose risks, such as HIV and hepatitis viruses. These measures are in place to safeguard both the recipient’s health and maintain donor confidence in the safety of the donation process.
Quality Assurance
The process of quality assurance encompasses comprehensive checks of collected blood units. These rigorous evaluations ensure that the blood supply remains free from contaminants and potential infections, reinforcing the integrity of transfusion practices. The adherence to strict quality protocols helps reinforce public trust, encouraging more donations and ensuring patient safety.
Encouraging Donations
Despite the constant need, the volume of donations can fluctuate based on several factors, including how well the public understands and supports the significance of regular blood donations. Initiatives aimed at education and advocacy are crucial in raising awareness and prompting an increase in the number of regular donors. These campaigns help underline the impact that regular donations have on saving lives.
How to Get Involved
By becoming regular donors, individuals contribute significantly to healthcare effectiveness. To embark on this compassionate journey, one can consult organizations like the American Red Cross or NHS Blood and Transplant for comprehensive information about the donation procedure and eligibility standards. They provide essential guidance on how best to prepare for a donation, establish the requirements you need to fulfill, and identify donation centers.
The role played by blood banks is undeniably foundational within the healthcare system. They ensure the blood supply is dependable and accessible for both routine healthcare needs and emergency situations. A sustained effort in donor recruitment and adherence to stringent safety measures underscores their critical function, ensuring that these invaluable resources are efficiently utilized.